 Case Report
Case Report
Isolated Intracranial Rosai-Dorfman Disease: A Diagnostic Challenge
Harsh Patel*, Preeti Singh and Abhaya Kumar
Department of Neurosurgery, Kokilaben Dhirubhai Ambani Hospital & Research Institute, India
Harsh Patel, Department of Neurosurgery, Kokilaben Dhirubhai Ambani Hospital & Research Institute, Mumbai, India.
Received Date:August 30, 2024; Published Date:September 13, 2024
Abstract
Isolated intracranial Rosai-Dorfman disease (RDD) is an extremely rare, idiopathic histoproliferative disorder. RDD is associated with the proliferation of histiocytes and emperipolesis. RDD radiologically mimics meningioma and dural metastasis as dural-based lesions and histologically mimics plasma cell granuloma, langerhans cell histiocytosis (LCH) and lymphoproliferative disease. Central nervous system (CNS) involvement is extremely rare and due to rarity of RDD, it is not usually proposed in intracranial lesions diagnosis. RDD can occur at any age but is more commonly noted in adolescents. Typical presentation is with massive cervical lymphadenopathy alongside features of a raised erythrocyte sedimentation rate, anemia, pyrexia, and polyclonal hypergammaglobulinemia.2 Extranodal manifestations occur in ≈43% of cases, although central nervous system involvement is present in <5% of cases.2,3 RDD has a prevalence of 1 in 200,000 and an estimated incidence of 100 new cases per year in the United States.4 Isolated intracranial disease is rare and can easily be mistaken for other pathologies due to similarities of imaging characteristics We report a case with isolated intracranial RDD. A 47-year- old man presented with focal seizure. This case preoperatively was misdiagnosed with meningioma. Histopathological examination revealed pale histiocytes displaying emperipolesis which were positive for S-100 and CD68 proteins and negative for CD1a marker. BRAF V600E mutation was negative. In this case, total resection was performed and clinical symptoms were regressed completely.
Case Summary
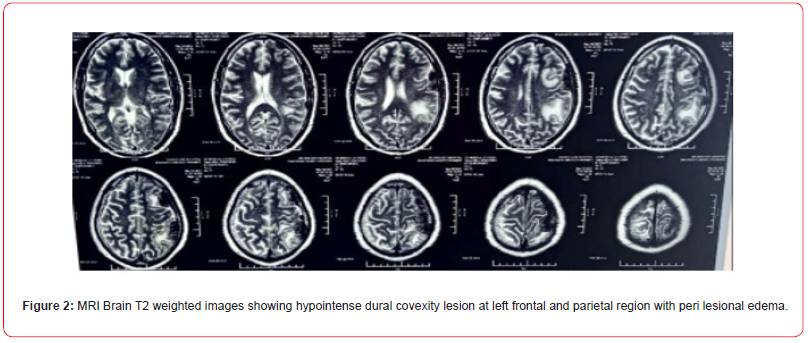
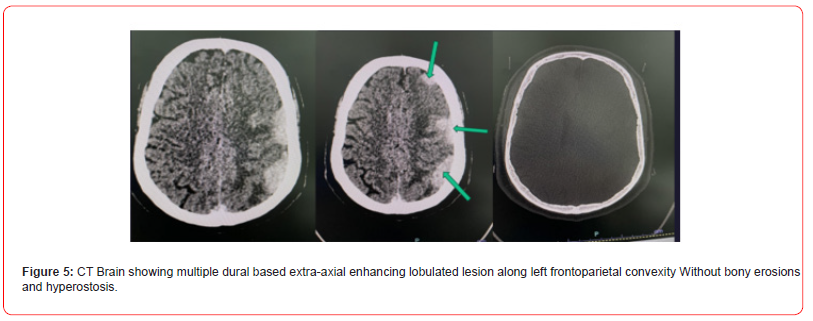
A 47 year male presented in Department of Neurosurgery with chief complaints of focal seizure involving right side of face and right upper limb with tingling sensation in right upper limb from 1 year. 5 to 6 episodes of focal seizure per day lasting for 40-50 secs was present. Patient consulted many neurologist who started him on multiple antiepileptic drugs but there was no relief. There was no history of trauma, incontinence, altered speech, memory alteration, visual impairment, vertigo and childhood seizure. On examination right hand grip weakness was present. Rest of the examination was unremarkable. Further radiological investigations were done (Figure 1 to 5).
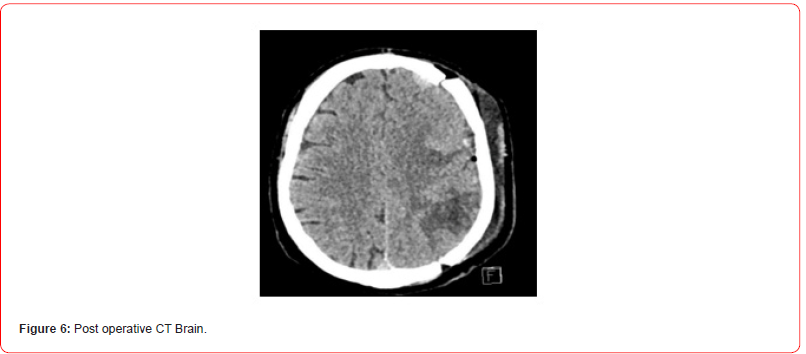
Clinical and radiological diagnosis of en-plaque meningioma of left frontoparietal convexity compressing the underlying parenchyma was made. Patient was planned for craniotomy and surgical excision of lesion. Intraoperatively after removing the calvarium at left fronto -parietal aspect. Dura was visible with some nodular lesions underneath it. On opening the dura we found three lesions lying over cortical surface of parietal and frontal lobes, yellowish nodular oval shaped well defined lesions attached with dura with no clear demarcation/plane of dissection between lesion and brain tissue. Suspecting some high grade lesion en mass excision was done except the part of nodule present over middle frontal gyrus which was in proximity of pial vessel to avoid pial violation. Tissue sample was sent for histopathological examination. On post operative day 3 patient had an episode of focal seizure in right hand. CT brain was done which showed patchy edema in the subcortical white matter in the left parietal lobe , involving the postcentral gyrus and to a lesser extent the left frontal lobes with few foci of hemorrhage. No increase in mass-effect since preoperative study. No significant midline shift or brainstem herniations (Figure 6).
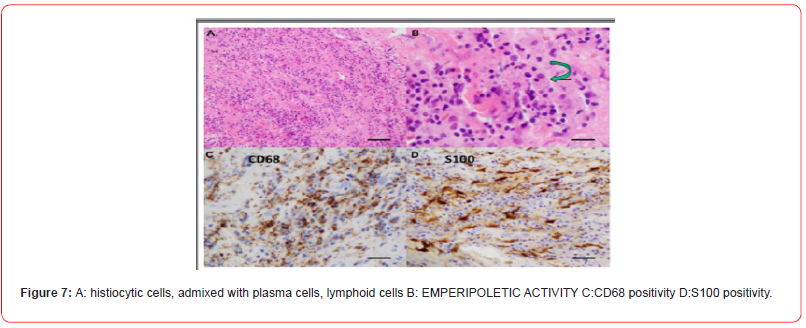
Histopathological examination shows histiocytic cells, admixed with plasma cells, lymphoid cells, emperipoletic activity, CD68 positivity suggestive of IgG4 related hypertrophic pachymeningitis. Tissue blocks were reviewed which showed pale histiocytes displaying emperipolesis which were positive for S-100 and CD68 proteins and negative for CD1a marker. BRAF V600E mutation was negative rosai dorfman disease (Figure 7).
Post operative period was uneventful with no episodes of focal seizures and improvement in right hand grip. Patient antiepileptic medication and low dose steroid was continued. Whole body PET CT was negative except Solitary FDG uptake in left frontal lobe area. Antiepileptic medication was continued and steroids were gradually tapered and stop. Patient was advised to follow up after 3 months with repeat MRI Brain.
Discussion
Rosai-Dorfman-Destombes disease (RDD) is a rare histiocytic disorder described by Destombes in 1965 and later by Rosai and Dorfman in 1969 as ‘sinus histiocytosis with massive lymphadenopathy’ and previously classified by the Working Group of the Histiocyte Society of 1987 as a non langerhans cell (LC) histiocytosis. It is a benign self-limiting condition characterized by the accumulation of activated histiocytes in the sinusoids of lymph nodes and/ or extranodal tissues.1 Classic RDD presents with massive bilateral painless cervical lymphadenopathy with associated fever, loss of weight and night sweats. Extranodal disease is seen in over 40% of cases and may rarely occur in the absence of nodal disease, usually in older patients with different demographics. It predominantly affects children and young adults, but the disease can be seen in the range of 1 to 74 years old. Common extranodal sites of involvement include the skin (10%), nasal cavity (11%),bone (5%–10%),orbital tissue (11%) central nervous system (5%, predominantly dural):mostly involving the two sides of the dura and mimicking meningioma. 2 They can occur in the suprasellar region, convexity, parasagittal region, cavernous sinus, petroclival region and cerebellum. CNS Rosai-Dorfman disease shows a predilection for males, and typically presents during the 4th to 5th decade with the mean age of 39.4 years old.3 The definitive diagnosis is based on histopathological examination and immunohistochemistry. RDD can be misdiagnosed with different isotypes of meningioma and other en plaque dural lesions.
Conclusion
Intracranial variety of RDD is very rare (5%) , although rare it may lead to serious complications like blindness and deafness. So early and accurate diagnosis is very important. Extranodal RDD, especially isolated intracranial RDD as shown in the present case, may pose a diagnostic challenge both for the clinician, radiologist and the pathologist as radiological and clinical features mimics like en plaque meningioma. Clinically, as do meningiomas, intracranial Rosai-Dorfman disease causes a variety of clinical symptoms depending on lesion location. Thus headache, epilepsy, cranial nerve deficits, and various other symptoms may be seen or become evident with disease progression. Frequent lesion locations include the cerebral convexities, the parasagittal, suprasellar, and cavernous sinuses, and petroclival regions Definitive diagnosis primarily relies on histopathological examination of biopsy tissue (emperipolesis, CD68, S100 staining), and resection of the intracranial mass is the most effective treatment for intracranial RDD. When neurologic symptoms persist or there are lesions around vital structures, the implementation of adjuvant therapies is recommended, together with localized radiotherapy. To explain regarding close follow up to the patient is very important as chances of recurrence is 14-29 %. RDD should be differentiated from IgG4 related disease as well .11 IgG4 related disease responds very well with corticosteroids alone. Histologically, it is characterized by an attenuated infiltration of lymphoplasmacytic cells and histiocytes of varying sizes. The large, pale histiocytic cells contain what looks like engulfed lymphocytes (“emperipolesis”) within their cellular borders 12. Immunophenotype S100: positive, CD11c: positive, CD68: positive, L1 antigen: positive, CD1a: negative. Radiographic features due to the wide disease spectrum, radiographic features can be variable. Nodal involvement is appreciated as lymphadenopathy on plain film and cross-sectional imaging. In CT it is seen as hyperattenuating meningeal-based mass showing contrast enhancement. and parenchymal edema surrounding the lesion may be present. In MRI meningeal-based masses which appear isointense to grey matter in T1, hypointense to grey matter in T2 and homogeneous enhancement in T1 C+ (Gd). Nuclear medicine often shows increased uptake with gallium scanning and increased metabolism with FDG-PET. Treatment and prognosis Rosai-Dorfman disease usually follows a benign and self-limiting course with treatment largely targeted at controlling local manifestations (surgical intervention) 6. The pathologic differential diagnosis of this particular case included lymphoma, plasma cell granuloma, and Langerhans cell histiocytosis. Lymphoma was unlikely, considering the lack of monotonous atypical lymphocytes. It may be difficult to distinguish Rosai-Dorfman disease from plasma cell granules in the absence of emperipolesis (lymphocytophagocytosis); previous reports of plasma cell granuloma encompassed both entities. Our preliminary, frozen section diagnosis was plasma cell granuloma. Langerhans cell histiocytosis was unlikely because Langerhans histiocytes with their familiar folded nuclei and eosinophil infiltrates were absent, as was immunoreactivity for CD1a, a reliable marker of Langerhans cell histiocytosis. Intracranial Rosai-Dorfman disease has been treated with surgery or other methods involving steroids, chemotherapeutic agents, and radiation. Among these treatments, the surgical resection seems to be the most effective. The prognosis of Rosai- Dorfman disease with involvement of the CNS was not poor. In a review of follow-up data of 43 patients, most patients (58%) were alive with disease. Only two patients (4.7%) had died . Moreover, no death was reported to have occurred as a result of isolated intracranial Rosai-Dorfman disease. Although Rosai-Dorfman disease is a rare process, it should be included in the differential diagnoses for a dural mass mimicking meningioma. Furthermore, we should remember that Rosai-Dorfman disease may show an unusual imaging pattern, as it did in this case at the time of first presentation. Although neuroradiology might be of aid in the diagnosis of isolated intracranial Rosai-Dorfman disease, only histopathologic and immunocytochemical examinations permit a firm diagnosis.
Acknowledgement
None.
Conflict of Interest
No Conflict of interest.
References
- O Abla, et al. (2018) Consensus recommendations for the diagnosis and clinical management of Rosai-Dorfman-Destombes disease. Blood.
- H Zhu, et al. (2012) Imaging characteristics of Rosai-Dorfman disease in the central nervous system. Eur J Radiol.
- Pirko, et al. (2009) Deep gray matter T2 hypointensity correlates with disability in a murine model of MS J Neurol Sci.
- Y Jiang, et al. (2018) Intracranial meningeal Rosai-Dorfman disease mimicking multiple meningiomas: 3 case reports and a literature review. World Neurosurgery.
- Andriko JA, Morrison A, Colegial CH, et al. (2001) Rosai-Dorfman disease isolated to the central nervous system: A report of 11 cases. Mod Pathol 14: 172–8. [PubMed] [Google Scholar]
- Cheng-Hong Toh, Yao-Liang Chen, Ho-Fai Wong, et al. (2005) Rosai—Dorfman disease with dural sinus invasion Report of two cases. J Neurosurg 102: 550–554. [PubMed] [Google Scholar]
- Deodhare SS, Ang LC, Bilbao JM (1998) Isolated intracranial involvement in Rosai- Dorfman disease.A report of two cases and review of the literature. Arch Pathol Lab Med 122:161–5. [PubMed] [Google Scholar]
- Andriko JA, Morrison A, Colegial CH, Davis BJ, Jones RV (2001) Rosai-Dorfman disease isolated to the central nervous system: a report of 11 cases. Mod Pathol 14: 172–178
- Kattner KA, Stroink AR, Roth TC, Lee JM (2000) Rosai-Dorfman disease mimicking parasagittal meningioma: case presentation and review of literature. Surg Neurol 53:452–457
- Huang HY, Huang CC, Lui CC, Chen HJ, Chen WJ (1998) Isolated intracranial Rosai-Dorfman disease: case report and literature review. Pathol Int 48: 396–402
- Wu M, Anderson AE, Kahn LB (2001) A report of intracranial Rosai-Dorfman disease with literature review. Ann Diagn Pathol 5: 96–102
- Kitai R, Sato K, Kubota T, et al. (1996) Meningeal sinus histiocytosis mimicking lymphoplasmacyte-rich meningioma. J Neurosurg 84: 1051–1054
- Deodhare SS, Ang LC, Bilbao JM (1998) Isolated intracranial involvement in Rosai-Dorfman disease: a report of two cases and review of the literature. Arch Pathol Lab Med 122: 161–165
-
Harsh Patel*, Preeti Singh and Abhaya Kumar. Isolated Intracranial Rosai-Dorfman Disease: A Diagnostic Challenge. Arch Neurol & Neurosci. 17(1): 2024. ANN.MS.ID.000904.
-
Acute Polyradiculoneuritis, Neurology, Guillain-barre; Fann teaching hospital, neuropathy, cranial nerves, immunotherapy, Neuroscience, neurogenic syndrome, epidemiological, Dysphonia.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






